Healthy Community
Vision: In 2040, Roanoke engages a holistic and equitable approach to building and ensuring the physical and mental health of our community by empowering citizens with the knowledge and resources to achieve healthy living and to strive for accountability as individual members of a connected society.
Introduction
Community health is a complex issue, one that has not been addressed in past planning efforts. City Plan 2040 considers wellness in its most broad sense and explores how safety and security, poverty, transportation systems, housing, access to food, and access to support services interrelate in ways that shape the health of the community.
In addition to supporting health at the individual level, agencies interested in improving community health work to influence the conditions that affect health outcomes. These conditions are identified as the social determinants of health. The US Department of Health and Human Services defines social determinants of health as the environmental conditions “that affect a wide range of health, functioning, and quality-of-life outcomes and risks” and organizes them into the five domains identified in the graphic below.
As with Interwoven Equity, policies that address the social determinants are embedded in every theme of this plan. Community health has an inextricable link with equity because of neighborhood-level disparities in social determinants like transportation, housing, land use, local economy, the built environment, and so on. Accordingly, planners worked to integrate policy ideas to influence social determinants of health in a positive direction, particularly those within the Economic Stability and Neighborhood and Built Environment domains. The Healthy Community theme directs some of the specific interventions that work within the Health Care Access and Quality and Social and Community Contextdomains.
Health in All Policies
As we developed City Plan 2040, City staff and partners participated in the Change Lab Solutions’ Building Healthy, Equitable Communities for Children & Families project. This technical assistance project shaped thinking about community health and underscored the importance of considering all the different factors that influence health. Singular focus on a particular factor doesn’t yield the desired improvement in overall community health. The idea that we need to press all the levers of influence at once has spurred progressive communities to adopt a health in all policies approach. Because city planning is so policy oriented, it is appropriate to consider the health in all policies approach as we develop ideas among the different themes of this plan.
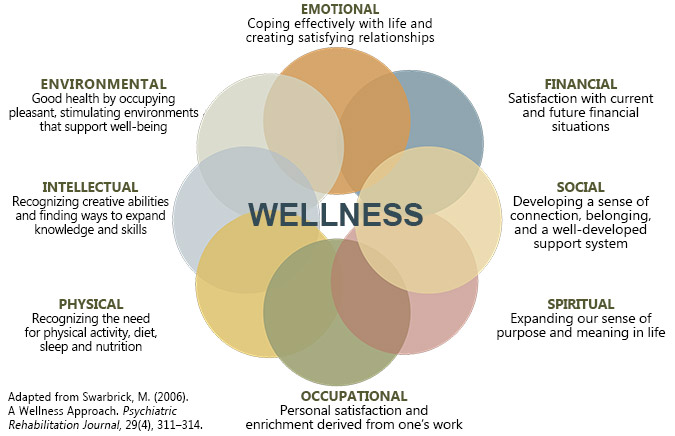
Wellness
A holistic view of wellness is needed to assess community health and develop corresponding public policy. The Department of Health and Human Services identifies eight dimensions of health and wellness. Physical health related to exercise, nutrition and rest is the most recognized of these element. Physical health, along with the other elements of emotional, financial, social, spiritual, occupational, intellectual, and environmental health form an interconnected state of wellness. Lack of security in any of these areas can lead to impacts to mental or physical health.
Some of these elements are largely addressed within this theme while other aspects, such as financial and environmental health are largely addressed in other theme area. This demonstrates the breadth of public health concerns.
The social and emotional components of wellness can be more difficult to identify and then address, and have a lasting effect on a person’s overall wellbeing. Approaching these elements requires a proactive and lasting approach, beginning at an early age. The U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration has extensive tools and resources on multi-pronged, trauma-informed approaches to addressing health issues. The trauma-informed approach recognizes how violence, abuse, neglect, loss, and other emotionally harmful experiences impact health.
The social and emotional components of wellness can be difficult to identify and address than the physical ones. Because of their lasting effect on a person’s overall wellbeing, approaching these elements requires persistent and deliberate attention, beginning at an early age. The U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration has extensive tools and resources on multi-pronged, trauma-informed approaches to addressing health issues. The trauma-informed approach recognizes how violence, abuse, neglect, loss and other emotionally harmful experiences impact health.
When it comes to physical health, obesity and chronic disease, are serious problems in our communities – in some more than others. Chronic diseases, influenced in large part by tobacco use, alcohol abuse, lack of exercise, and poor diet, affect 6 in 10 adults and are a leading cause of death and disability in the U.S. Some 80% of health outcomes are determined by people’s behavior, environment, or social and economic conditions. As might be expected, health outcomes vary widely by neighborhood based upon social and economic conditions.
More recently, mental health and substance abuse issues have gained attention, particularly with the opioid epidemic, highlighting the need for more holistic discussions about health.
Safety
During the listening phase of the planning process, Roanoke residents discussed how transportation, infrastructure, law enforcement, and a sense of community influence community safety and feelings of security. Residents identified safety as both a strength and a challenge for the community. This sentiment was further emphasized in the Healthy Community working group discussions that recognized important linkages between security and health. For example, regular exercise is a key building block of health, and walking is the easiest form of exercise available to most people. But what if people don’t feel safe going for a walk in their neighborhood or worry about their personal security when they go to a park? Safe Wise’s “State of Safety” reports that 58% of Americans are concerned about their safety at some point of every day. We are all familiar with priorities of preventing safety hazards and preventing crime, but actual and perceived safety can also be created with infrastructure like sidewalks, crosswalks, and bike accommodations on streets.
Safewise Reported Level of Daily Safety Concern (U.S. %)
Safe and Healthy Homes
Good housing is key determinant of good health outcomes. It is important to not just have access to housing, but healthy housing. While most of Roanoke’s housing is well-maintained and healthy, some housing units are not. Census data indicates that about 4% of Roanoke’s housing is substandard and lacks complete plumbing or kitchen facilities. Roanoke’s Office of Real Estate Valuation identified 431 structures that are in poor or very poor condition.
Environmental hazards in some of Roanoke’s older housing stock can be a challenge. Over 80% of homes were built before 1979 and, while historic homes add to the character of the city, some have the potential for lead based paints, asbestos and other materials that are now recognized as health hazards. Until updated, older houses may not have electrical systems suitable for modern appliances or other structural or maintenance issues that represent potential safety hazards.
The Building Safety Division, the Code Enforcement Division work to improve housing conditions. Improving home and building safety includes consideration of age of housing stock, sanitation, other health risks such as mold, lead and asbestos, and hazards related to building systems (e.g., wiring) to which renters and low-income individuals are especially vulnerable. Community Resources Division through housing rehabilitation projects and programs like Lead SAFE Roanoke have eliminated environmental hazards in hundreds of homes.
Age of Roanoke Housing Stock (U.S. Census)
Access to Health and Support Services
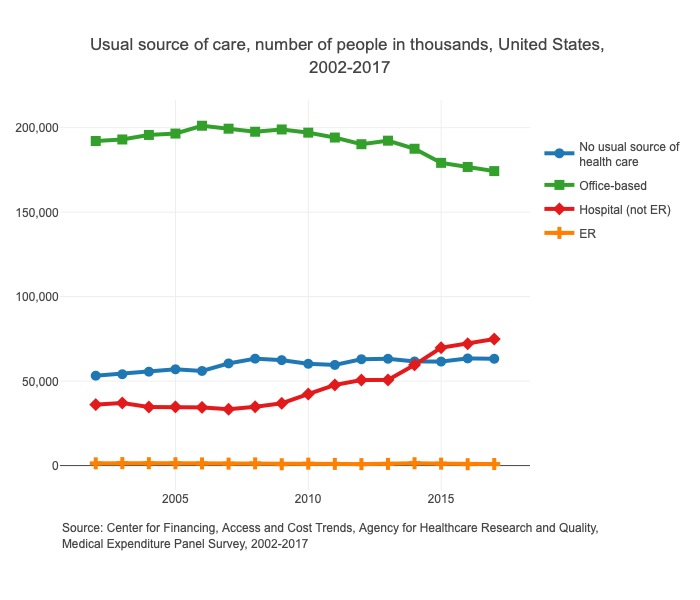
The percentage of uninsured Americans has increased; 8.5% of people lacked health insurance in 2018. Coinciding with the increase in uninsured individuals, the Medical Expenditure Panel Survey shows that office-based health care is on the decline and the number of people relying on hospitals as a source of care has increased.
While the recent expansion in Medicare has aimed to fill these gaps and has provided new access for approximately 9,000 Roanoke residents, access to health care is still an issue for varying reasons, including high cost, inadequate insurance coverage, lack of availability of services, poor provider trust, and lack of culturally competent care. Removing barriers like these would create more equitable access.
Lack of access to services health and support services can be even more pronounced for those that are homeless or those that suffer from mental health or substance abuse issues. In addition to barriers associated with cost, insurance, and availability, there is an added barrier to access related to siting facilities. People frequently object to treatment or care facilities in their neighborhoods. The equity dimension can be complicated. Facilities are needed and they need to be accessible and they need to be distributed throughout the city.
Access to Affordable Healthy Food
The Kroger and Mick-or-Mack stores that once bristled with activity in neighborhoods like Melrose and Belmont disappeared in the 1990s. Before then, people had the choice to walk or drive to get their weekly groceries. These stores were replaced, however, with larger stores in shopping centers near the outskirts of town. Located far from any residences, they are accessible only by car or bus. Meanwhile, large neighborhood areas are left with no access to groceries within the community. Despite strong community support to attract grocery stores back to neighborhoods, there is little indication that will happen given the scale and markets required. Public intervention in some form may be needed to address this issue.
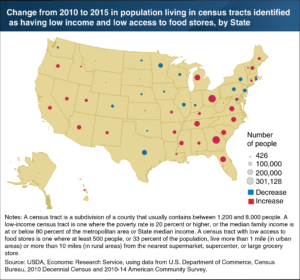 Suburbanization of grocery stores has led to so-called food deserts in urban neighborhoods. Food deserts lead to food insecurity. The Oxford Dictionary defines food insecurity as “The state of being without reliable access to a sufficient quantity of affordable, nutritious food.” In 2018, 11% of U.S. households experienced food insecurity. Particularly, Virginians have seen a marked increase in the number of low-income individuals with low access to food stores. While many residents are able to drive to pick up groceries, this is especially difficult for vulnerable populations such as low-income people, children, and seniors. Food insecure households are more likely to shop at convenience stores, where healthy food choices are rare or nonexistent.
Suburbanization of grocery stores has led to so-called food deserts in urban neighborhoods. Food deserts lead to food insecurity. The Oxford Dictionary defines food insecurity as “The state of being without reliable access to a sufficient quantity of affordable, nutritious food.” In 2018, 11% of U.S. households experienced food insecurity. Particularly, Virginians have seen a marked increase in the number of low-income individuals with low access to food stores. While many residents are able to drive to pick up groceries, this is especially difficult for vulnerable populations such as low-income people, children, and seniors. Food insecure households are more likely to shop at convenience stores, where healthy food choices are rare or nonexistent.
Health Equity
Perhaps the most important observation about community health is how it varies among different populations. Many of the health factors above merge to create remarkably different health outcomes from one community to another. We see inequity in patterns in life expectancy and disease rates among different neighborhoods, and this is where issues of health and equity intersect. Equitable health outcomes should be the ultimate goal. All policy and action should be oriented to reducing these inequities.
Priority One: Wellness
The National Wellness Institute recognizes that “wellness is a conscious, self-directed and evolving process of achieving full potential”, in addition to being “multidimensional and holistic, encompassing lifestyle, mental and spiritual well-being, and the environment”. Achieving this priority requires policies that address each of the many aspects of wellness.
Priority Two: Safety
Communities in which residents feel safe and comfortable create an environment where residents can be active, healthy, and thriving.
Priority Three: Access to Health and Support Services
In order to improve access to health care and resulting health outcomes, barriers to health services need to be reduced.
Priority Four: Access to Affordable Healthy Food
Feeding American calculates that over 16% of Roanoke residents are food insecure. Public-private partnerships must be strengthened in order to remove barriers to food equity and find innovative solutions for improving access and health education.
Introduction
Community health is a complex issue, one that has not been addressed in past planning efforts. City Plan 2040 considers wellness in its most broad sense and explores how safety and security, poverty, transportation systems, housing, access to food, and access to support services interrelate in ways that shape the health of the community.
In addition to supporting health at the individual level, agencies interested in improving community health work to influence the conditions that affect health outcomes. These conditions are identified as the social determinants of health. The US Department of Health and Human Services defines social determinants of health as the environmental conditions “that affect a wide range of health, functioning, and quality-of-life outcomes and risks” and organizes them into the five domains identified in the graphic below.
As with Interwoven Equity, policies that address the social determinants are embedded in every theme of this plan. Community health has an inextricable link with equity because of neighborhood-level disparities in social determinants like transportation, housing, land use, local economy, the built environment, and so on. Accordingly, planners worked to integrate policy ideas to influence social determinants of health in a positive direction, particularly those within the Economic Stability and Neighborhood and Built Environment domains. The Healthy Community theme directs some of the specific interventions that work within the Health Care Access and Quality and Social and Community Contextdomains.
Health in All Policies
As we developed City Plan 2040, City staff and partners participated in the Change Lab Solutions’ Building Healthy, Equitable Communities for Children & Families project. This technical assistance project shaped thinking about community health and underscored the importance of considering all the different factors that influence health. Singular focus on a particular factor doesn’t yield the desired improvement in overall community health. The idea that we need to press all the levers of influence at once has spurred progressive communities to adopt a health in all policies approach. Because city planning is so policy oriented, it is appropriate to consider the health in all policies approach as we develop ideas among the different themes of this plan.
Wellness
A holistic view of wellness is needed to assess community health and develop corresponding public policy. The Department of Health and Human Services identifies eight dimensions of health and wellness. Physical health related to exercise, nutrition and rest is the most recognized of these element. Physical health, along with the other elements of emotional, financial, social, spiritual, occupational, intellectual, and environmental health form an interconnected state of wellness. Lack of security in any of these areas can lead to impacts to mental or physical health.
Some of these elements are largely addressed within this theme while other aspects, such as financial and environmental health are largely addressed in other theme area. This demonstrates the breadth of public health concerns.
The social and emotional components of wellness can be more difficult to identify and then address, and have a lasting effect on a person’s overall wellbeing. Approaching these elements requires a proactive and lasting approach, beginning at an early age. The U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration has extensive tools and resources on multi-pronged, trauma-informed approaches to addressing health issues. The trauma-informed approach recognizes how violence, abuse, neglect, loss, and other emotionally harmful experiences impact health.
The social and emotional components of wellness can be difficult to identify and address than the physical ones. Because of their lasting effect on a person’s overall wellbeing, approaching these elements requires persistent and deliberate attention, beginning at an early age. The U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration has extensive tools and resources on multi-pronged, trauma-informed approaches to addressing health issues. The trauma-informed approach recognizes how violence, abuse, neglect, loss and other emotionally harmful experiences impact health.
When it comes to physical health, obesity and chronic disease, are serious problems in our communities – in some more than others. Chronic diseases, influenced in large part by tobacco use, alcohol abuse, lack of exercise, and poor diet, affect 6 in 10 adults and are a leading cause of death and disability in the U.S. Some 80% of health outcomes are determined by people’s behavior, environment, or social and economic conditions. As might be expected, health outcomes vary widely by neighborhood based upon social and economic conditions.
More recently, mental health and substance abuse issues have gained attention, particularly with the opioid epidemic, highlighting the need for more holistic discussions about health.
Safety
During the listening phase of the planning process, Roanoke residents discussed how transportation, infrastructure, law enforcement, and a sense of community influence community safety and feelings of security. Residents identified safety as both a strength and a challenge for the community. This sentiment was further emphasized in the Healthy Community working group discussions that recognized important linkages between security and health. For example, regular exercise is a key building block of health, and walking is the easiest form of exercise available to most people. But what if people don’t feel safe going for a walk in their neighborhood or worry about their personal security when they go to a park? Safe Wise’s “State of Safety” reports that 58% of Americans are concerned about their safety at some point of every day. We are all familiar with priorities of preventing safety hazards and preventing crime, but actual and perceived safety can also be created with infrastructure like sidewalks, crosswalks, and bike accommodations on streets.
Safewise Reported Level of Daily Safety Concern (U.S. %)
Safe and Healthy Homes
Good housing is key determinant of good health outcomes. It is important to not just have access to housing, but healthy housing. While most of Roanoke’s housing is well-maintained and healthy, some housing units are not. Census data indicates that about 4% of Roanoke’s housing is substandard and lacks complete plumbing or kitchen facilities. Roanoke’s Office of Real Estate Valuation identified 431 structures that are in poor or very poor condition.
Environmental hazards in some of Roanoke’s older housing stock can be a challenge. Over 80% of homes were built before 1979 and, while historic homes add to the character of the city, some have the potential for lead based paints, asbestos and other materials that are now recognized as health hazards. Until updated, older houses may not have electrical systems suitable for modern appliances or other structural or maintenance issues that represent potential safety hazards.
The Building Safety Division, the Code Enforcement Division work to improve housing conditions. Improving home and building safety includes consideration of age of housing stock, sanitation, other health risks such as mold, lead and asbestos, and hazards related to building systems (e.g., wiring) to which renters and low-income individuals are especially vulnerable. Community Resources Division through housing rehabilitation projects and programs like Lead SAFE Roanoke have eliminated environmental hazards in hundreds of homes.
Age of Roanoke Housing Stock (U.S. Census)
Access to Health and Support Services
The percentage of uninsured Americans has increased; 8.5% of people lacked health insurance in 2018. Coinciding with the increase in uninsured individuals, the Medical Expenditure Panel Survey shows that office-based health care is on the decline and the number of people relying on hospitals as a source of care has increased.
While the recent expansion in Medicare has aimed to fill these gaps and has provided new access for approximately 9,000 Roanoke residents, access to health care is still an issue for varying reasons, including high cost, inadequate insurance coverage, lack of availability of services, poor provider trust, and lack of culturally competent care. Removing barriers like these would create more equitable access.
Lack of access to services health and support services can be even more pronounced for those that are homeless or those that suffer from mental health or substance abuse issues. In addition to barriers associated with cost, insurance, and availability, there is an added barrier to access related to siting facilities. People frequently object to treatment or care facilities in their neighborhoods. The equity dimension can be complicated. Facilities are needed and they need to be accessible and they need to be distributed throughout the city.
Access to Affordable Healthy Food
The Kroger and Mick-or-Mack stores that once bristled with activity in neighborhoods like Melrose and Belmont disappeared in the 1990s. Before then, people had the choice to walk or drive to get their weekly groceries. These stores were replaced, however, with larger stores in shopping centers near the outskirts of town. Located far from any residences, they are accessible only by car or bus. Meanwhile, large neighborhood areas are left with no access to groceries within the community. Despite strong community support to attract grocery stores back to neighborhoods, there is little indication that will happen given the scale and markets required. Public intervention in some form may be needed to address this issue.
 Suburbanization of grocery stores has led to so-called food deserts in urban neighborhoods. Food deserts lead to food insecurity. The Oxford Dictionary defines food insecurity as “The state of being without reliable access to a sufficient quantity of affordable, nutritious food.” In 2018, 11% of U.S. households experienced food insecurity. Particularly, Virginians have seen a marked increase in the number of low-income individuals with low access to food stores. While many residents are able to drive to pick up groceries, this is especially difficult for vulnerable populations such as low-income people, children, and seniors. Food insecure households are more likely to shop at convenience stores, where healthy food choices are rare or nonexistent.
Suburbanization of grocery stores has led to so-called food deserts in urban neighborhoods. Food deserts lead to food insecurity. The Oxford Dictionary defines food insecurity as “The state of being without reliable access to a sufficient quantity of affordable, nutritious food.” In 2018, 11% of U.S. households experienced food insecurity. Particularly, Virginians have seen a marked increase in the number of low-income individuals with low access to food stores. While many residents are able to drive to pick up groceries, this is especially difficult for vulnerable populations such as low-income people, children, and seniors. Food insecure households are more likely to shop at convenience stores, where healthy food choices are rare or nonexistent.
Health Equity
Perhaps the most important observation about community health is how it varies among different populations. Many of the health factors above merge to create remarkably different health outcomes from one community to another. We see inequity in patterns in life expectancy and disease rates among different neighborhoods, and this is where issues of health and equity intersect. Equitable health outcomes should be the ultimate goal. All policy and action should be oriented to reducing these inequities.
Priority One: Wellness
The National Wellness Institute recognizes that “wellness is a conscious, self-directed and evolving process of achieving full potential”, in addition to being “multidimensional and holistic, encompassing lifestyle, mental and spiritual well-being, and the environment”. Achieving this priority requires policies that address each of the many aspects of wellness.
Priority Two: Safety
Communities in which residents feel safe and comfortable create an environment where residents can be active, healthy, and thriving.
Priority Three: Access to Health and Support Services
In order to improve access to health care and resulting health outcomes, barriers to health services need to be reduced.
Priority Four: Access to Affordable Healthy Food
Feeding American calculates that over 16% of Roanoke residents are food insecure. Public-private partnerships must be strengthened in order to remove barriers to food equity and find innovative solutions for improving access and health education.